As a breast cancer surgeon, I’ve long been alarmed at the infiltration of non-evidence-based treatments that have steadily been infiltrating the specialty of oncology under the guise of “integrative oncology.” Indeed, I just realized that it’s been a full decade since I managed to publish a rather long opinion piece in Nature Reviews Cancer, in which I questioned whether integrative oncology is truly, as its proponents advertise, “the best of both worlds.” (Even if they haven’t actually read the article, regular readers will readily guess what my answer to that question was. Hint: Think Betteridge’s law of headlines.) It’s also been a decade since the primary “professional” organization representing “integrative oncology,” The Society for Integrative Oncology (SIO) published a monograph that supposedly presented “evidence-based” guidelines for the specialty. (Hint: They weren’t evidence-based.) Meanwhile, here at SBM I’ve written a number of posts discussing how, unlike the vision of its proponents of combining the “best of both worlds” (science-based medicine and “holistic”/alternative medicine) for the betterment of patient care, in reality what integrative oncology does, just as the more general “specialty” of “integrative medicine” under which it falls does, is to combine unproven and disproven treatments that include even outright quackery and mysticism with conventional, boring science-based oncology while simultaneously “rebranding” accepted evidence-based interventions involving diet and lifestyle as somehow being “alternative” or “integrative,” rather than just medicine.
I mention this background because last week, while perusing the journals that I like to peruse to see what’s new in cancer research and oncology, I came across a commentary published in Nature Reviews Cancer by three heavy hitters (if you can call them that) in integrative oncology, Gabriel Lopez, Santhosshi Narayanan, and Lorenzo Cohen, entitled Integrative medicine in oncology: redefining the standard of care. Oddly enough, it was about a decade ago when I attended a meeting of the American Society of Clinical Oncology (ASCO) in which Lorenzo Cohen PhD, a prominent proponent of integrative oncology at the University of Texas M.D. Anderson Cancer Center, promoted various “mind-body” woo as part of a panel talk, particularly yoga and a “wishing makes it so” idea more subtle than German New Medicine. He’s also featured in this blog a number of times before dating back to 2008 for overselling his acupuncture studies in cancer patients, for example. When I saw this article, I realized that, clearly, here was some blog fodder. Let’s dig in.
“Redefining the standard of care”?
The authors state their purpose right in the abstract:
Integrative medicine incorporated alongside cancer care, referred to as integrative oncology, is an evidence-informed field with established clinical guidelines. Although integrative oncology improves patient outcomes, it is inconsistently provided to patients. To align with best practices, it is necessary to increase awareness of integrative oncology, improve access to treatments, and provide consistent financial healthcare coverage.
I do like the careful choice of words here. Notice how the authors refer to integrative oncology as “evidence-informed,” rather than “evidence-based.” The wag in me can’t resist suggesting that evidence might “inform” integrative oncology, but that integrative oncology’s “integration” of quackery like acupuncture rather suggests to me that that “informing” was largely ignored in favor of ideology. I was also very interested in the assertion that integrative oncology improves patient outcomes, as I am unaware of any high quality scientific evidence that it does anything of the sort. The best that I’m aware of is that in the hands of practitioners who are less ideological, view themselves as more evidence-based, and try to act accordingly integrative oncology probably doesn’t harm patients. Probably. Of course, that’s in contrast with the more—shall we say?—avid proponents of integrative oncology who eagerly team up with naturopaths and practitioners of traditional Chinese medicine (TCM), deluding themselves that this improves patient care.
Notice, also, the framing. The authors view integrative oncology as an unalloyed good, a cutting edge concept that, because it’s so new, is “inconsistently provided to patients.” Because the authors view their specialty as an advancement over boring old conventional oncology, they view lack of access to modalities like TCM and acupuncture, reflexology, and the like as a health care disparity that must be urgently addressed. All cancer patients must have access to TCM, acupuncture, and all the other non-evidence-based treatments that integrative oncology has to offer! The authors even lament this disparity in more detail in the opening paragraph:
The goal of integrative oncology is to provide comprehensive support to individuals with cancer, their caregivers and their family across the cancer care continuum. According to the Journal of the National Cancer Institute expert consensus definition, integrative oncology is: “a patient centered, evidence-informed field of cancer care that utilizes mind and body practices, natural products, and/or lifestyle modifications from different traditions alongside conventional cancer treatments. Integrative oncology aims to optimize health, quality of life, and clinical outcomes across the cancer care continuum and to empower people to prevent cancer and become active participants before, during, and beyond cancer treatment”1. In the USA, most National Cancer Institute (NCI)-designated Comprehensive Cancer Centers now have integrative oncology programs that enable access to this coordinated approach in conjunction with their oncology care plan. However, owing to inconsistent healthcare coverage, limited institutional funding, and lack of awareness for integrative oncology services, only a minority of patients have access to and/or utilize these treatments. Outside the USA, integrative oncology services are even more inconsistently provided to patients. This is equally true for high-, middle- and low-income countries. Yet some countries such as China, South Korea and Japan have integrative oncology often seamlessly integrated within the healthcare system.
I discussed the expert consensus definition of integrative oncology referred to above. In particular, I noted what the definition left out, namely just how quacky the modalities “integrated” into oncology in the specialty can be, including how the SIO admits naturopaths and even elects them as the organization’s president from time to time, never mind that all naturopaths are trained in The One Quackery To Rule Them All, homeopathy, and that the vast majority of naturopaths routinely prescribe homeopathic remedies, which, even the SIO concedes, are rooted in pseudoscience. It also leaves out how the SIO is fine with “integrating” quackery such as reflexology, reiki, and acupuncture into oncology and doesn’t object to even homeopathy at UC-Irvine and the Cleveland Clinic. At the University of Arizona Cancer Center, there was reiki, at least until a faculty member whose child developed cancer and was treated there made a stink. There’s also more energy medicine quackery, this time in the chemotherapy suite, at Georgetown University, as well as cupping, which is also pure quackery. There’s functional medicine at the Cleveland Clinic, George Washington University, University of Kansas, and, well, seemingly almost everywhere at any medical center with an integrative medicine program. If you want an idea of how bad functional medicine is, just check out this case report of functional medicine used for a patient with inflammatory breast cancer. This is what integrative oncology really involves.
As for why China, South Korea, and Japan have what the authors view as successful “integrative oncology,” one only has to understand the strong cultural affinity in such countries for the various forms of traditional Asian medicine, which is often “integrated” into the healthcare system. This is particularly true in China, where the government retconned the history of TCM and how it was promoted by Chairman Mao Zedong as both a substitute for “Western medicine” when he did not have enough physicians and as a cultural triumph of China to export to the world, the latter a message eagerly taken up by credulous journalists. In addition, China has used its influence with the World Health Organization (WHO) to “integrate” TCM diagnoses into the ICD-11 and promote TCM as “evidence-based,” even as it has actively promoted TCM as an industry whose products it exports to the world while requiring it in state hospitals, lowering the bar for its approval, passing laws to protect TCM against criticism—or what it calls “slandering” or “libeling” TCM—and even forcing its citizens to use TCM to treat COVID-19 early in the pandemic. Such is the largest of the systems that the authors admire because of its “seamless” integration of “traditional medicine” with medicine. Funny how the authors are unaware of this history or intentionally didn’t mention it.
But back to the touted “evidence base,” which is mentioned many times in the commentary, starting with the SIO guidelines, which are supposedly rooted in scientific and clinical evidence:
As the discipline of integrative oncology has expanded, there is a better understanding of how best to support patients using an integrative approach that may include counselling on different topics and various integrative oncology treatments. There is now an extensive research base that spans the methodology from observational studies using patient-reported outcomes to randomized clinical trials that assess symptom control and more objective outcomes. The field has matured to such an extent that there are now several organizations developing integrative oncology clinical practice guidelines.
There are also several organizations that represent naturopaths and acupuncturists. This is not a good argument. Also, as I’ve long discussed, generally most of the evidence for the therapies “integrated” into oncology (and medicine) are observational, and the relatively few randomized controlled clinical trials that exist are inevitably, when examined critically, negative, suffer from fatal methodological flaws, or tout minimal effects that are clinically irrelevant. (Advocates love to do this, in particular, for studies of acupuncture, such as this one.) Acupuncture, of course, is one of the most prominent “traditional” therapies that advocates like the authors love to “integrate” into oncology.
Unfortunately, the authors aren’t wrong when they note how totally embedded “integrative oncology” has become in mainstream oncology organizations:
The American Society of Clinical Oncology (ASCO) endorsed the SIO guidelines in 2018 and both organizations now have a formal partnership to co-develop multiple guidelines for the use of integrative oncology in cancer care including for pain management2, anxiety and depression2, and fatigue2 with sleep guidelines under development. Similarly, the National Comprehensive Cancer Network (NCCN) guidelines recommend using integrative therapies to treat several cancer- related and cancer treatment-associated symptoms. A summary of these recommendations is provided in Table 1. Integrative oncology contributes in substantial ways to symptom management in cancer care. Combinations of integrative oncology therapies may be considered to address several symptoms. Some integrative oncology therapies may be recommended despite the lower quality of evidence if there is some evidence for efficacy and a high safety profile. For example, patients living in a remote area may not have access to acupuncture but may be able to practice yoga for relief of aromatase inhibitor-induced arthralgia, although there is less evidence for yoga than for acupuncture.
I had to chuckle at that last sentence. “Less evidence for yoga than for acupuncture”? That would seem to imply that there is negative evidence for yoga, given that there is basically zero evidence for acupuncture against aromatase inhibitor-induced joint pain, as I discussed when deconstructing the study most commonly cited to support the use of acupuncture for this indication, including its update that tried—but failed—to provide evidence that acupuncture actually does work for aromatase-induced arthralgias.
As for Table 1, let’s take a look:
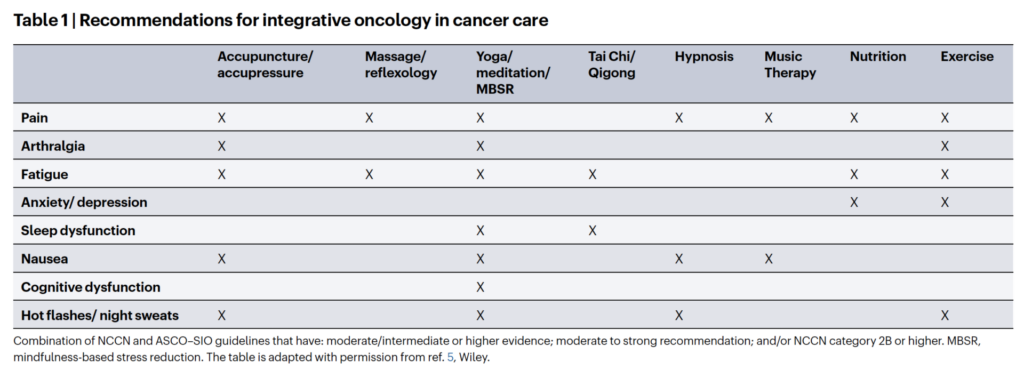
Reference 5 is a 2022 review article touting integrative oncology as a means to address global challenges of cancer treatment and prevention, and the table above is basically a rehash of that two-year-old table, which was basically a rehash of a previous 2021 article on supportive care in oncology. Let’s just say that none of the evidence for acupuncture for any of these indications is particularly strong;. Taken in totality, the evidence is actually most consistent with acupuncture being a theatrical placebo. Moreover, when you look critically at the studies touted by advocates, you will nearly always find that the RCTs at least are, in actuality, negative studies. Indeed, seeing acupuncture listed as having at least moderate quality evidence in the table makes me suspicious of everything else in the table. I won’t belabor the point too much, but, once again, I discussed the RCTs commonly cited for acupuncture for arthralgia and hot flashes in depth years ago. They were negative studies.
Amusingly, the authors (sort of) concede one of my big points about “integrative oncology,” namely that a lot of cancer centers are a bit more—shall we say?—expansive in their definition of what is “evidence-based”:
Some centres closely follow the clinical practice guidelines and avoid providing interventions that are not on the guidelines (such as Reiki), whereas others are more liberal with incorporating herbs or other modalities within their practice model. The more liberal approach can have downsides, including adverse events and the perception within the conventional oncology community that integrative oncology uses a different standard of evidence before incorporating a treatment as the standard of care outside of the research setting. This highlights the need for robust research efforts and more funding support for conducting integrative oncology clinical trials.
The “more liberal” approach? I laughed when I read this. After all, the whole idea of “integrative” oncology (or medicine) is to erase the boundaries between quackery and science-based medicine. Personally, of course, we at SBM have long argued for one standard of evidence, the science-based standard, to be applied to all medical interventions and tests. That’s why I was also amused at how unhappy the authors are about the perception that integrative oncology “uses a different standard of evidence.” It’s not just perception. As much as authors like Lorenzo Cohen like to try to shoehorn modalities like acupuncture into oncology as somehow being just as “evidence-based” as any other treatment in oncology, when you come right down to it, they are still just “integrating” quackery into oncology and throwing a patina of seeming EBM on top of it to hide the incredibly implausible nature of many of the “integrative” interventions touted, including in TCM. The standard of evidence for “integrative” therapies gets a much lower bar to clear than conventional, particularly pharmaceutical, treatments.
Putting the cart before the horse
As is nearly always the case with advocates for “integrating” unscientific treatments with science-based treatments, the authors cheerfully argue for putting the cart before the horse and pushing to “integrate” quackery with oncology, all in the name of…battling health disparities and disparities in access to care, which (of course) includes persuading third party payors to fund their woo:
As the evidence has grown in support of integrative oncology interventions, more healthcare insurers have begun to include these interventions as covered services. Yet, coverage is inconsistent. To mitigate growing healthcare disparities, it is crucial for all healthcare systems and insurers to align with the evidence and include integrative oncology treatments delineated in the clinical care guidelines within the standard of care. In addition, third-party payors need to be consistent across regions in terms of what is covered (for example, coverage of acupuncture should not depend on the state or province you live in but on medical evidence)
I’ll actually agree with that last sentence, although, unlike what the authors think, applying such a standard in my estimation would mean that third party payors should not cover acupuncture at all in their health insurance plans. I’d say the same thing for reflexology, TCM, and naturopathy (again, a prominent component of SIO to the point where two of the group’s past presidents have been naturopaths, even though the SIO downplays its relationship with naturopaths). In any event, just as those touting all forms of “integrative medicine” always do, the authors are putting the cart before the horse, advocating the adoption of prescientific and scientifically implausible theatrical placebos like acupuncture before there is strong evidence that they are efficacious for anything, all while claiming that “integrative oncology” has advance so much and become so evidence-based—excuse me, “evidence-informed”:
Integrative oncology as a field has advanced tremendously through the ever-expanding evidence-base. Although in many countries integrative oncology is provided in coordination with conventional oncology care to improve symptom control, quality of life, psychosocial wellbeing and clinical outcomes, there are many inconsistencies and most patients still lack access to these guideline-based, evidence-informed treatments. To improve patient outcomes, it is necessary to increase awareness of these treatments, provide more training of oncology and integrative clinicians on offering only evidence-informed services, and expand coverage for treatments by payors. In this way, integrative oncology will be more seamlessly incorporated within the standard of care.
I would question whether integrative oncology has advanced at all as a field in the decade since SIO first published its “guidelines.” How can it when the vast majorities of the modalities that it seeks to “integrate” are not science-based and the ones that can plausibly claim a basis in science and clinical evidence (e.g., nutrition) have been taken from medicine and “rebranded” as somehow “alternative” or “integrative”? As we at SBM have long argued, there really should be no such thing as “integrative” medicine, because medicine should be by default “integrative” in that it will integrate treatments that have been shown through science and rigorous clinical investigation to be safe and effective, to the point that “integrative” is an unnecessary addition to the word “medicine.”

